I’m a therapist, and I hear “I’m fine” all the time. Sometimes it’s said with a shrug and a smile; other times it’s practically whispered. I’ve even caught myself saying it when I don’t mean it. We use “I’m fine” as a reflex—brushing off pain or worry so we don’t burden others, or because we hope if we say it enough, it’ll become true. But behind those two little words often lies a quiet storm of stress, hurt, or exhaustion. And the hidden cost of “I’m fine” is far higher than we like to admit.
Putting on a brave face
On the surface, saying you’re fine keeps the peace. You seem strong, low-maintenance, “handling it.” But inside, unresolved feelings don’t just disappear; they simmer. You keep juggling work deadlines, family needs, social obligations—telling everyone (and yourself) it’s fine. The result is often a slow build-up of quiet burnout.
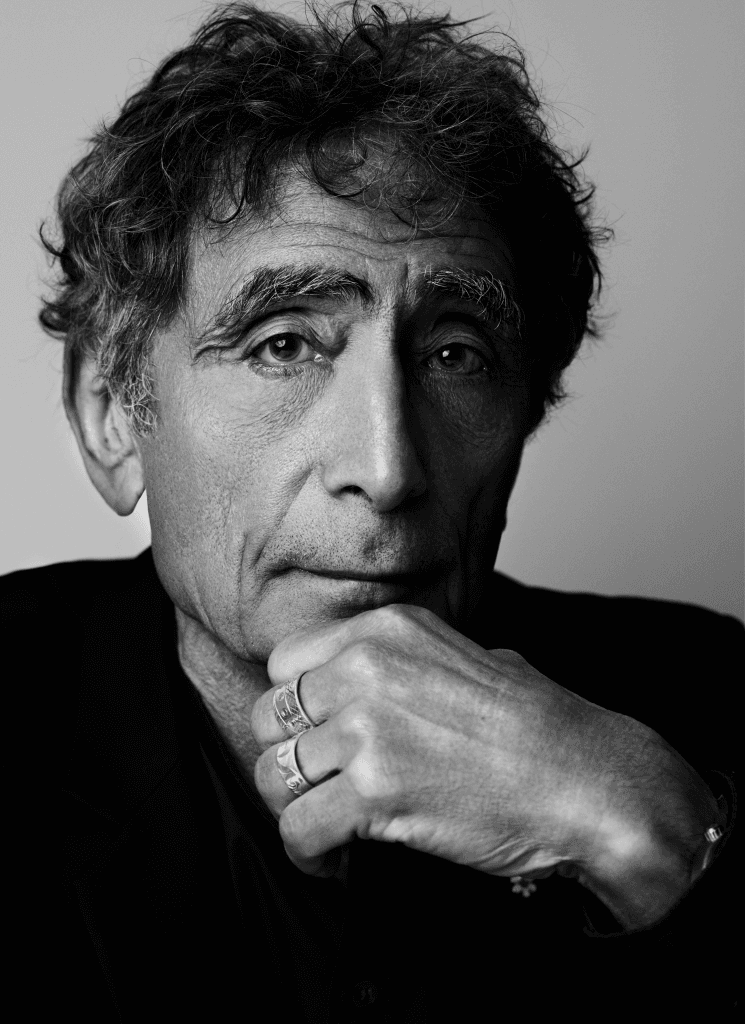
As physician Gabor Maté has observed, “It takes tremendous energy to suppress emotions. The act itself is stress producing.” In other words, bottling up our feelings doesn’t make them go away. It just forces our bodies and minds to carry a heavier load.
And that load shows up in ways we might not immediately connect to stress. Maybe your fine is turning into frequent tension headaches or an irritable gut. Maybe “I’m fine” looks like snapping at your partner or kids over tiny things (and feeling terrible after). We say we’re okay to avoid appearing weak or dramatic, but inside the pressure is building. The longer we keep up the “I’m fine” act, the heavier that lie becomes, and the harder it feels to finally say “I’m not okay.” Quietly, our mental and emotional health erode. We edge closer to burnout, even as we keep smiling on the outside.
The slow burn of suppressed stress
When distress is downplayed for too long, it often leads to a kind of slow-motion burnout. No one wakes up one day and instantly burns out—it’s more like a candle melting down, silently.
If you’ve ever had a stretch where you’re doing everything “right” yet feel empty or constantly drained, that’s the slow burn I’m talking about. High-functioning anxiety and quiet depression often hide behind “I’m fine.” Over time, this can progress to what one client of mine termed “functional burnout”—you’re technically coping, but joy has flatlined and every task feels herculean.
The World Health Organization actually recognizes burnout as a syndrome resulting from chronic workplace stress, and more broadly, untreated anxiety or depression can wear us down to the point of serious impairment. In fact, depression is now a leading cause of ill health and disability worldwide. That’s not just a statistic—it means countless people dragging themselves through days, saying they’re fine while their quality of life quietly crumbles.
We pay a price in productivity and creativity, too. The brain fog sets in; motivation tanks. The hidden cost isn’t just personal either—it ripples out. Globally, untreated mental health issues like depression and anxiety result in an economic loss of about $1 trillion in lost productivity every year. It’s staggering to consider, and it underscores that so many of us are suffering in silence, trying to push through. Eventually, something gives. It might be a health scare, a breakdown at work, or a relationship crisis that forces a reckoning. My hope is that we can take the exit ramp before we crash.
When “I’m fine” strains relationships
There’s another cost to the “I’m fine” routine: our relationships. When you constantly insist you’re okay, the people who care about you are left in the dark. Your partner senses something’s off but hears “I’m fine.” Your friends ask if you’re alright, you smile and say “totally!” – and they take you at your word.
Over time, this creates distance. As renowned couples therapist Esther Perel notes, when one partner stays silent about their inner struggles, the other often experiences that silence as “avoidance and distance”. In one of Perel’s workshops, someone pleaded to their spouse, “I tell you everything; you share nothing with me!”. That heartbreak is real.
By constantly saying “I’m fine,” we think we’re sparing our loved ones worry or keeping the relationship positive. But intimacy is built on being known, really known, in our moments of weakness as well as strength. When you never allow yourself to say “actually, I’m not okay” to your partner or a close friend, you inadvertently erect a wall. They can’t support a struggle they don’t know exists. Instead, they might misinterpret your stress-irritability or withdrawal as disinterest or coldness. In romantic relationships, unspoken pain can breed resentment or misunderstandings. Your silence (meant to protect the relationship) ends up slowly eroding it.
When the body keeps saying no
We often convince ourselves that emotional suffering is “all in our head,” but the body has a way of revealing the truth. Chronic stress and suppressed emotions will eventually speak through the body if we ignore them. Maybe your doctor can’t find a medical reason for your constant fatigue, or your neck and shoulders feel like concrete every evening. You might get sick more often, or old injuries flare up. This is not your body “betraying” you—it’s desperately trying to signal that you’re not fine.
As one New York Times health piece put it, the mind and body form a two-way street: “What happens inside a person’s head can have damaging effects throughout the body.” In fact, an untreated mental illness can significantly increase the risk of becoming physically ill. We know, for example, that prolonged depression and anxiety can raise the risk of heart disease and weaken the immune system. In short, our bodies often say “no” when we insist “I’m fine.”
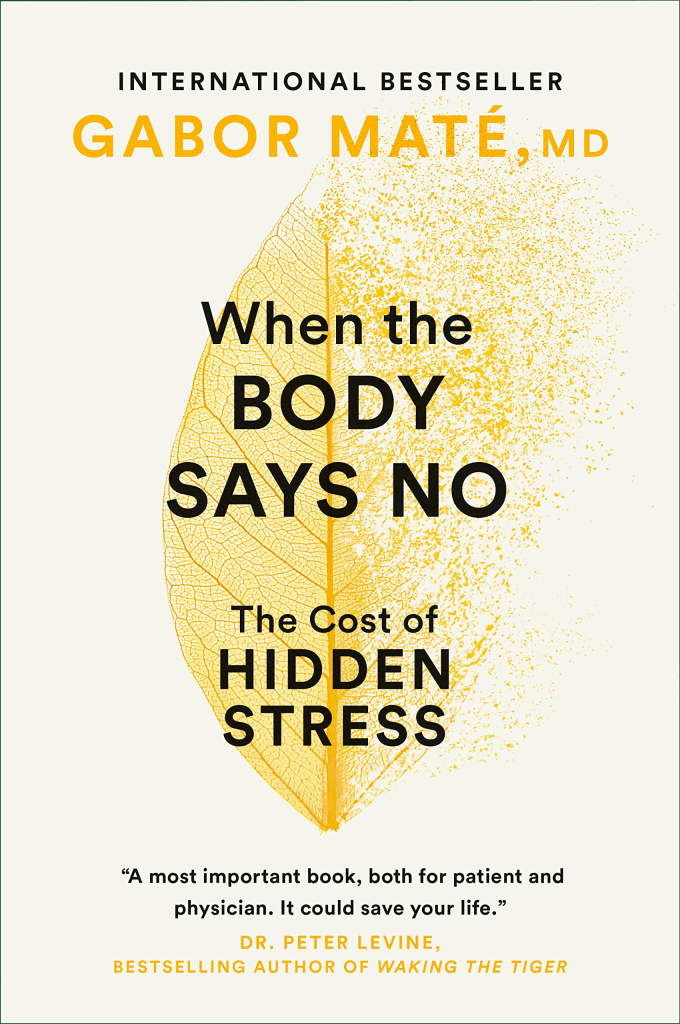
Gabor Maté, in his book When the Body Says No, documents case after case of people developing serious illnesses after years of chronically suppressing their needs and emotions. None of this means stress causes all illness (it doesn’t), but it’s a major risk factor we often underestimate. Our emotions will find a way to be heard, either through a healthy outlet or through burnout, breakdown, or physical symptoms.
Rather than viewing these symptoms as betrayal, we can view them as messages.
A panic attack, for instance, is your body’s alarm system saying “Something’s wrong – pay attention.” If we respond with “I’m fine, it’s nothing,” and push on, the alarm tends to get louder, whether in the form of more severe anxiety, deeper depression, or physical illness. Listening to your body’s signals without shame can be a powerful first step. It might be telling you that rest is needed, or that that unspoken grief or anger needs addressing.
Why we downplay our struggles
If saying “I’m fine” is so costly, why do we keep doing it?
- Stigma + early conditioning: Many of us were taught that big feelings = “dramatic” or “too sensitive,” so we downplay pain to avoid judgment.
- Gender scripts: Men get “real men don’t talk about feelings.” Women get “be the strong one, keep it together.” Either way: silence.
- Comparison trap: “Others have it worse, so I should be fine.” Pain isn’t a competition—drowning in 7 feet vs. 20 feet is still drowning.
- Fear of fallout: Admitting “I’m not fine” can mean facing grief, anger, or change (job, relationship, identity). The unknown feels scarier than the miserable status quo.
- Don’t-want-to-burden-anyone mode: You’re the helper, the fixer. Letting people in feels like inconvenience—but being trusted usually deepens connection.
Bottom line: these reflexes are common, but they keep you stuck. Naming them is the first crack in the “I’m fine” armour.
Signs you’re not actually fine
Next question: How can you tell if you’ve been saying “I’m fine” a bit too automatically? Here are a few signs that, beneath the surface, things might not be so fine after all:
- Every day feels like a marathon: You wake up already weary. Basic tasks that used to be routine (making breakfast, commuting, answering emails) feel like monumental efforts. You might be surviving on caffeine and sheer willpower.
- Joy is hard to come by: Activities you used to enjoy now feel like chores. You socialize less, or when you do, you feel disconnected and find yourself faking a smile. You catch yourself saying “I’m just tired” to explain the numbness.
- Irritability and mood swings: Little frustrations set you off. Maybe you’re unusually short with your partner or kids, or you rage at minor inconveniences in traffic. Afterward, you feel guilt or wonder, “Where did that come from?”
- Physical signs of stress: Your body is sounding alarms. This could be frequent headaches, muscle tension, stomach issues, or trouble sleeping (waking up at 3 AM with your mind racing). Perhaps you’re getting sick more often or relying on alcohol/TV/food to unwind every night.
- Withdrawal and isolation: You find yourself pulling back from people. Texts go unanswered. You cancel plans more frequently. It’s not that you don’t want to see people, you just can’t muster the energy. And when someone asks how you’re doing, you automatically say “I’m fine,” even though part of you hopes they’ll hear the hesitation in your voice.
These are just a few red flags. If several of them sound familiar, it might be time to pause and reconsider that automatic “fine.” There’s no shame in recognizing these signs; in fact, it’s a brave and healthy thing to do.
Therapy: relief before things spiral
One of the saddest patterns I see is people coming to therapy after a major crisis that might have been preventable—after they’ve been put on leave for burnout, after a panic attack lands them in the ER. Often in our first session they’ll say, “I should have come sooner. I’ve been struggling for years but I kept telling myself I was fine.” If that resonates with you, I say this with zero judgment (truly): don’t wait. Good therapy is not about giving you an excuse to wallow or picking apart your childhood ad nauseam; it’s about providing a safe space to unload that heavy backpack of unspoken stuff you’ve been carrying, and figuring out better ways to cope.

An invitation to honesty (with yourself and others)
If any of this hits home for you, and you feel you might be ready for a real conversation about how you’re doing, I encourage you to reach out. Whether it’s a free conversation with me or another therapist, a chat with your doctor, or a heart-to-heart with a close friend, take that step. You’re not alone, and you don’t have to pretend to be fine anymore. Let’s find what feeling better really looks like for you.
(If you’d like to talk, I’m here. Feel free to book a chat and we can explore some next steps together—at your pace.)

